†
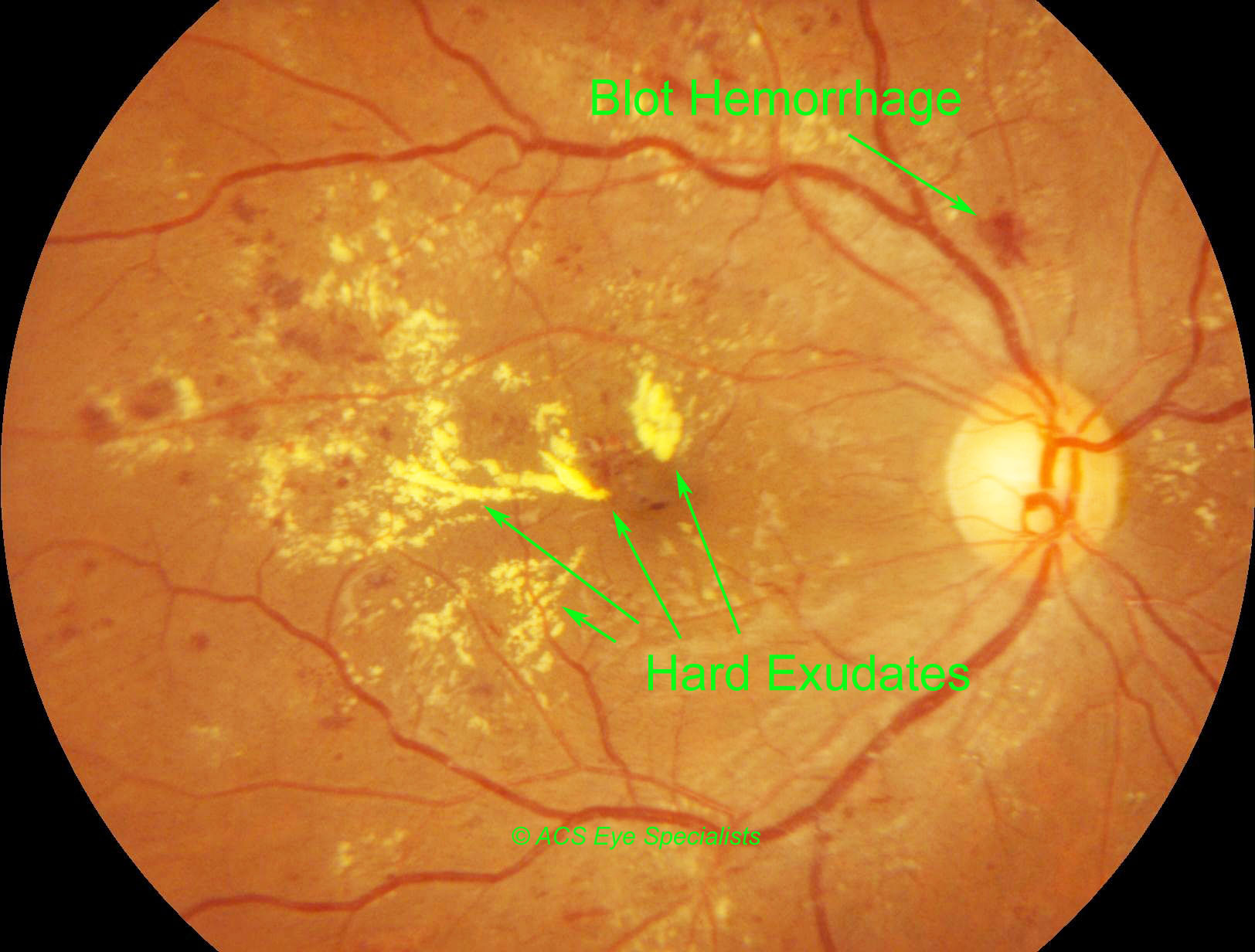
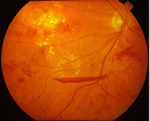
Hard Exudates in diabetic retinopathy
†
†
†
†
†

Diabetic Retinopathy
Diabetes is a disease that occurs when our body does not secrete enough insulin or is unable to process it properly. Insulin is the hormone that regulates the level of sugar (glucose) in the blood. Diabetes can affect both children and adults.
Overview
Diabetes is a disease that occurs when our body does not secrete enough insulin or is unable to process it properly. Insulin is the hormone that regulates the level of sugar (glucose) in the blood. Diabetes can affect both children and adults.How does diabetes affect the eye?
Patients with diabetes are more likely to develop eye problems such as cataracts and glaucoma, however the diseaseís effect on the retina is the main threat to vision. This is called diabetic retinopathy. Most patients develop diabetic changes in the retina after approximately 20 years.
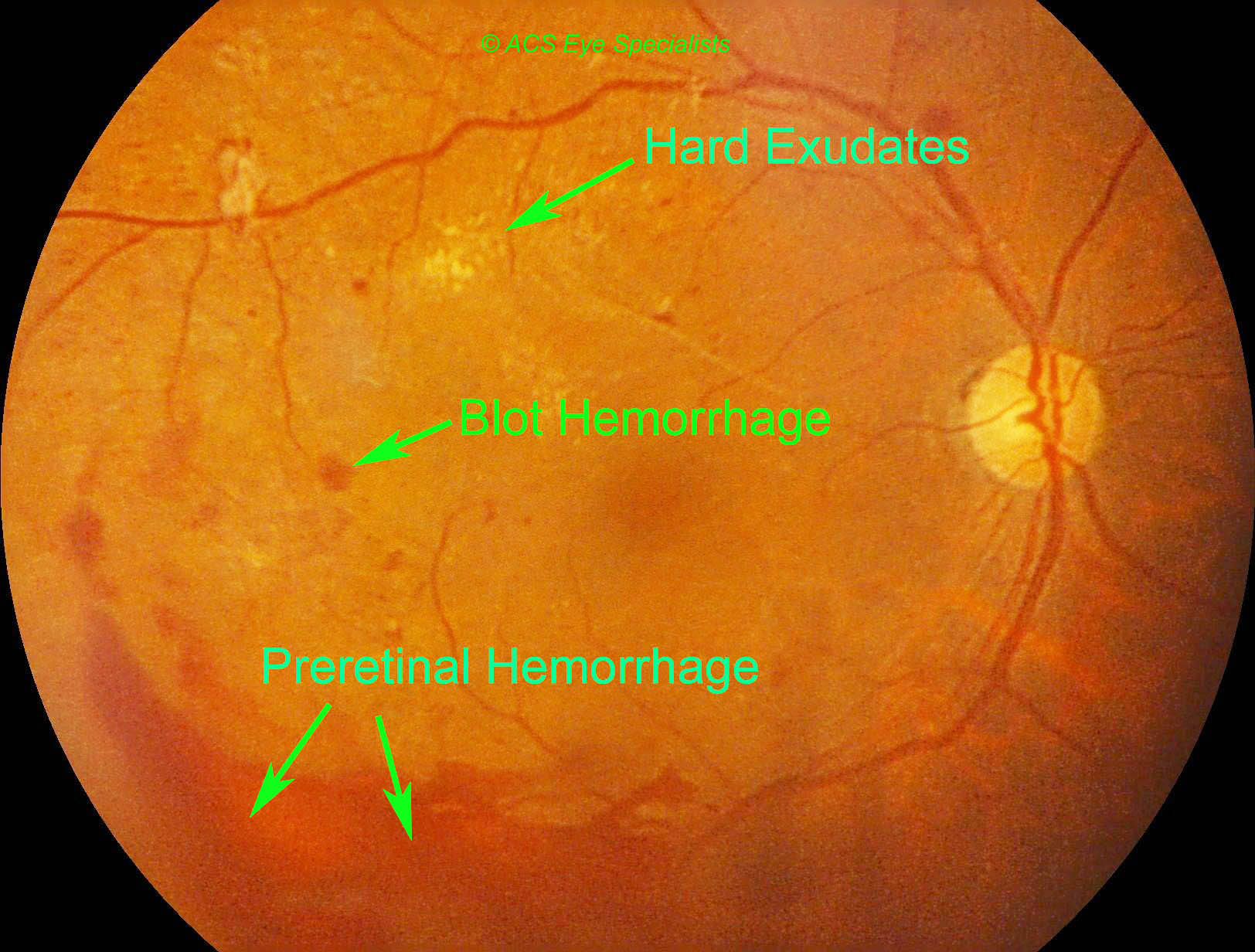
Over time, diabetes affects the vessels of the retina. The initial phase of the disease is known as nonproliferative diabetic retinopathy. Here, the arteries in the retina become weakened and leaky, causing small, dot-like hemorrhages. These leaking vessels often lead to swelling or edema in the retina and decreased vision. Your retina may also show cotton wool spots and hard exudates.
The next stage is known as proliferative diabetic retinopathy. In this stage, the lack of oxygen to the retina may cause certain areas of the retina to become oxygen-deprived or ischemic. As a result, fragile vessels grow in response to the lack of oxygen in an attempt to rectify the situation. This is termed as neovascularization. Unfortunately these vessels are very delicate and have the propensity to bleed easily. This can result in blood leaking into the retina and vitreous and cause a condition called floaters along with a reduction in vision.
If this condition is not controlled or treated, the continued abnormal vessel growth together with scar tissue formation will result in tractional retinal detachment and glaucoma.
What are the symptoms of Diabetic Retinopathy?
The effect of diabetic retinopathy on vision depends on the stage of the disease. Some of the symptoms include:
-
Blurred vision (this may fluctuate if it is linked to blood sugar levels)
-
Floaters and Flashes
-
Sudden loss of vision
How is Diabetic Retinopathy detected and diagnosed?
Diabetic patients require routine eye examinations so related eye problems can be detected and treated as early as possible. In order to detect any eye problems, diabetic patients should be examined by an ophthalmologist. The ophthalmologist will dilate your eyes following which a detailed examination will be made of your retina.There is new scanning "machine" called Optical Coherence Tomography (OCT) which is utilized to perform cross-sectional imaging of the retina. It facilitates measuring the macular thickening/oedema (swelling) and detecting abnormal pulling of the retina (vitreoretinal traction). Thus, OCT may assist in determining who needs treatment for Diabetic Retinopathy. Doctors can identify what treatment is required, and allow precise monitoring of treatment. It is useful for early detection and monitoring of Diabetic Retinopathy.
What is the treatment for Diabetic Retinopathy?
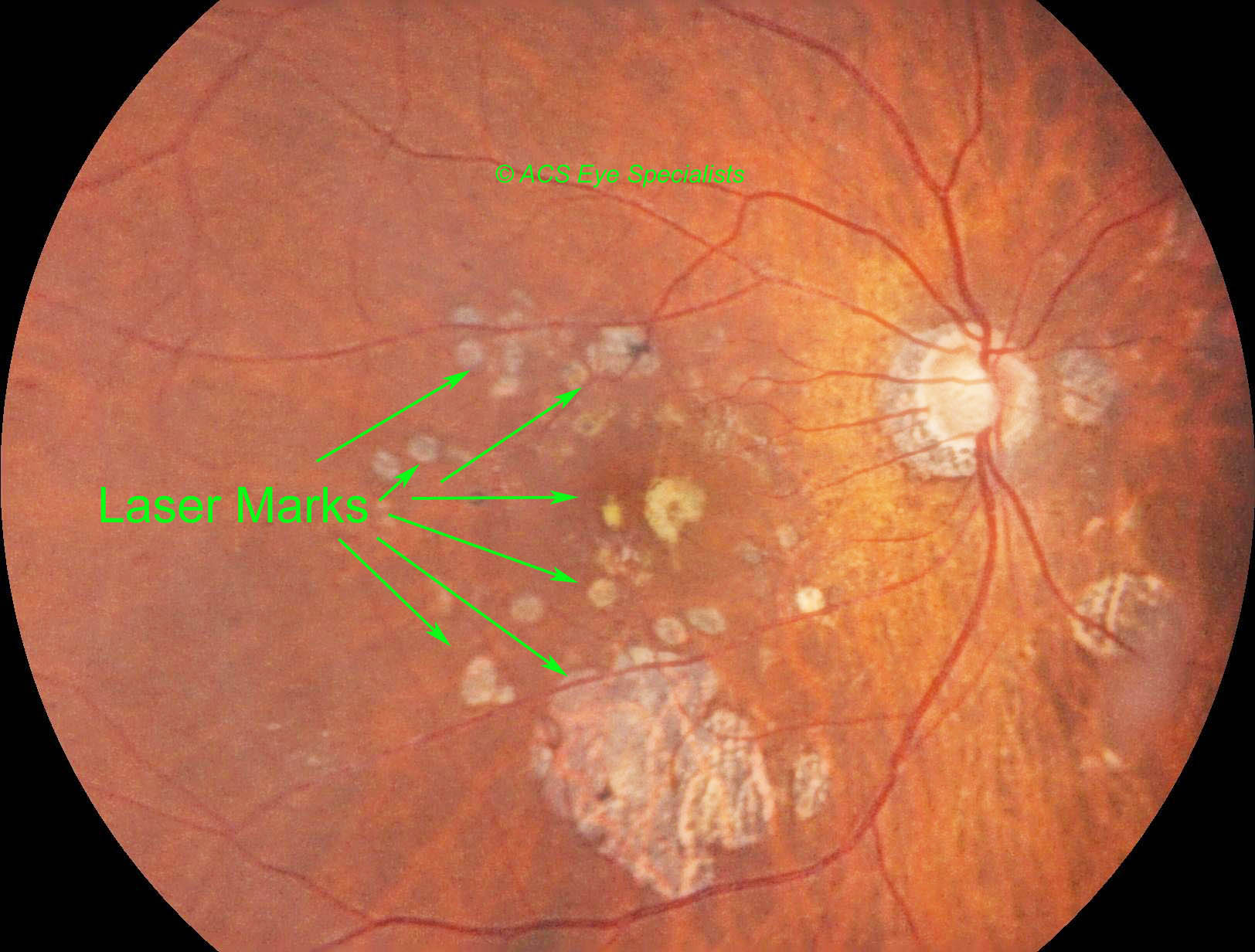
The treatment of diabetic retinopathy will depend on the stage of the disease and the specific problem that requires attention. Further investigations may be required to obtain more information about your eye. These include: fluorescein angiography, retinal photography, and ultrasound imaging of the eye.Initial treatment for the new vessels in the proliferative diabetic retinopathy stage is a laser treatment called pan retinal photocoagulation (PRP). In this procedure, the laser is used to destroy the oxygen deprived retinal tissue that is outside the patientís central vision. This helps to reduce the oxygen demand and thus will enable the abnormal new vessels to regress.
In advanced stages where laser PRP is unable to be performed such as in dense bleeding (vitreous hemorrhage), vitrectomy may be required to clear this bleeding in the gel-like substance that fills the center of the eye. During a vitrectomy, the surgeon carefully removes blood and vitreous from the eye, and replaces it with clear salt solution (saline). At the same time, any fibrous or scar tissue that is attached to the retina and can cause the pulling (traction) of the retina resulting in tears is also removed.
Untreated retinal traction in diabetic patients can result in the development of retinal tears and detachment. Tears are often sealed with laser treatment. Retinal detachment requires surgical treatment to reattach the retina to the back of the eye. The prognosis for visual recovery is dependent on the severity of the detachment.
Can I do anything to prevent Diabetic Retinopathy?
Researchers have found that diabetic patients who are able to maintain appropriate blood sugar levels have fewer eye problems than those with poor control. Diet and exercise play important roles in the overall health of those with diabetes.Diabetics can also greatly reduce the possibilities of eye complications by scheduling routine examinations with an ophthalmologist. Many problems can be treated with much greater success when caught early.